Wellbeing Erewash’s mission is to “develop thriving communities where people feel confident and supported to choose a healthier lifestyle, stay well, and know how to get help and support when they need it” and covers a population of 96,000. They aim to remove the boundaries that exist between organisations and give local people the information and confidence they need to support themselves.
One of the ways they are doing this is recruiting volunteer Community Connectors to work with individuals and groups in their communities to better understand what they need and how it can best be provided.
Community connectors are Wellbeing Erewash’s answer to what other services might call ‘care navigation’ or ‘community liaison’ officers. The difference here is that they are volunteers who spend their time in the community with a knowledge of what is the best locally available form of early intervention, regardless of organisational structures or budgets.
One of the Community Connectors Sharon told us “Since becoming partially sighted, I’ve seen how much connectors in the community can help support people. Becoming a Connector has given me more legitimacy and visibility to offer support and advice in my community. I’m working my way to build trust with people”. Sharon is now trained as a mental health first-aider and Dementia Friend, and has built up an in-depth knowledge of the local statutory and community services on offer in Erewash.
Sounds fluffy, does it work?
That there is insufficient evidence of short-term impact behind community-centred approaches for commissioners of public services to be persuaded to part with their dwindling resources in order to save on up-stream services, is an often cited barrier to taking community approaches to health.
Yet in 2016, Public Health England (PHE) attempted to call time on long-held assumptions that clinical interventions are the only way to improve health, and the only approaches which deserve significant funding.
Its then Chief Economist boldly stated: “No-one ever undertook a Randomised Control Trail to produce evidence of the cost-effectiveness of wearing seat belts in motor vehicles – yet the impact on population health has been enormous by any standards.”[1]
Analysis has time and time again shown that the NHS contributes only about 10-20% to overall population health[2]. Lifestyle-related behaviours, whether you have a good job and whether you have people around you that you can rely on is a far larger predictor of health outcomes.
Indeed, a “Health in All Policies (HiaP)”[3] approach, championed by the World Health Organisation as long ago as 1978, is quickly becoming mainstream with increased devolution of health and social care to Combined Authorities, as in Greater Manchester and the shifting of the responsibility for public health to local authority control.
From numbers to networks
In a recent workshop we heard the story of a largely immobile elderly person who took to walking to her local shop after the community transport services were cut, only to fall in the ice and require a hip replacement and long term care – costing immeasurably more to the NHS than it would if the council services were maintained.
Time and time again we see number crunching and short-termism fail to understand the power and the fragility of the connections, including services, which are necessary to keep us happy and healthy. As we’ve seen above, this approach leads us to make decisions that can prove counterproductive.
The RSA has a track record here. Our five year Connected Communities programme outlined a robust evidence base for the social return on investment through improving community connections. In its final report we highlighted that interventions such as Murton Mams, a peer to peer support group for young mothers (a group at heightened risk of social isolation) created dividends to the community that include improving subjective wellbeing to the mothers (50% increase in mothers feelings that the community included them) but also economic and social benefits to the people connected to the people involved in the intervention, including increased access to employment opportunities.
Making It Happen / Letting It Happen
The traditional model of public services instigates a top-down, hierarchical approach to the delivery of public services, which is more and more out of step with the model of “helping it happen” or “working with, not for” people that we advocate. We’ve seen these tensions in action.
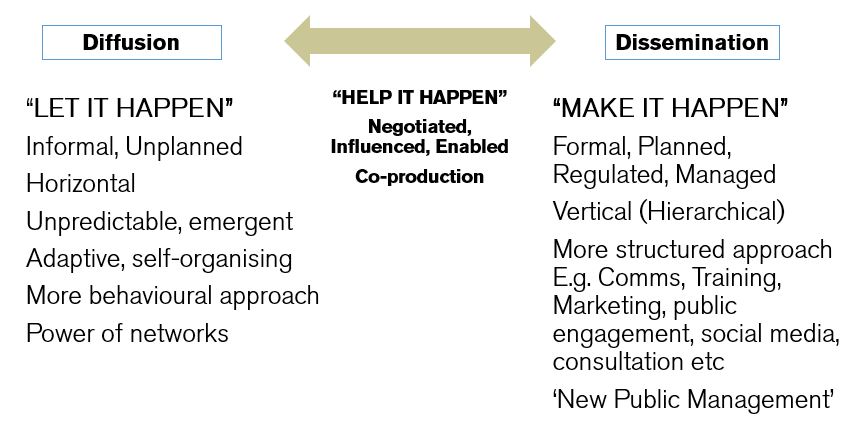
Source: The RSA Action and Research Centre
The well-trained, dedicated and energised Community Connectors in Erewash have to grapple with numerous consultants, evaluators and researchers (including ourselves) vying for their time. This pitting of the community-centred voluntary sector with the evaluation focused “make it happen” model mirrors a large gap in the rhetoric of healthcare leaders and policy makers and the reality on the ground.
We advocate for a middle ground in these approaches that sees the ‘restorative’ public services reinvigorated and trusted to “help it happen” and therefore secure long-term investment in prevention.
If you are interested in how you or your organisation could get involved with Wellbeing Erewash, please get in touch with Jo Hallam. If you live in Long Eaton, Erewash CVS is currently recruiting Community Connector volunteers.
If you have any queries about RSA’s work on the Health as a Social Movement programme, please contact Becca Antink.
Follow the author @_Tom_Harrison
[1] https://publichealthmatters.blog.gov.uk/2016/02/22/investing-in-prevention-the-need-to-make-the-case-now/
Related articles
-
A social justice cause for the 2020s – reining in health spending
Anthony Painter
Anthony Painter argues that the state expansionists will win over small statists as healthcare expenditure is destined to increase. But their victory may be a Pyrrhic one unless the growth can be limited so better support can also be given to housing, economic security, education and lifelong learning.
-
Did Bevan's bedpan test set the NHS on the wrong track?
Ed Cox
Ed Cox, Director of Public Services and Communities, argues that the NHS needs a more devolved approach in the decade ahead.
-
8 principles for future health and care systems
Tom Harrison
The RSA and NEF in partnership with NHS England publish eight principles to develop a community-led health system.



Join the discussion
Comments
Please login to post a comment or reply
Don't have an account? Click here to register.
Hi, I run a health and social care charity in Erewash and have been part of the Wellbeing Erewash project since its launch. We support many people in the community who have complex mental and / or physical health problems including those that are at end of life. We operate across Erewash supporting people who often reside in areas that are in the top 2.5% of social deprivation (IMD 2011). As an organisation we provide preventative services to help people to maintain their independence at home to keep them out of hospital and away from their GPs, we also help to get patients out of hospital quicker.
Whilst I agree that Community Connectors are a great way of keeping people up to date of which people and organisations can help, volunteers often only volunteer for a limited amount of time and so the project isn't sustainable. I also think a much bigger problem has been overlooked. There is a huge problem with 'e-government' within the community that I serve as many are poor, cannot afford technology and the older population aged 55+ are on the whole digitally excluded. Virtually everything is online and very little is printed. This means that for those who are considered 'hardest to reach' in the community - those that are housebound and digitally excluded - are isolated and disconnected from the rest of society. They have very little awareness of local services and consultations that may affect them.