GPs train for a minimum of seven years. In the workplace, up to 25% of their practice time relates to patients’ non-medical issues - requiring a different mind-set to that cultivated in training, where tools and approaches focus on clinical prescribing. We’ve been working with GPs in Morecambe Bay, finding new ways to relate more closely to people in their community to improve their health.
GPs face challenges from many directions. There has been a steady rise in patient expectations, a target driven culture and a growing requirement to accommodate work previously undertaken in hospitals, or in social care settings (GP Forward View).
The workload of GPs has grown both in volume and complexity, with a 15% increase in the number of consultations between 2010 and 2015. People are living longer while experiencing long-term health conditions, and while one in seven in the UK have serious long-term conditions, they account for half of all GP appointments.
New ways of working to upskill and embed prevention of illness are needed to address these challenges. The RSA in collaboration with the New Economics Foundation have been working with two visionary GPs in Morecambe and Barrow, working under the banner of the Better Care Together NHS vanguard, who are doing just that.

Better Care Together brings together two county councils (Lancashire and Cumbria), four NHS Foundation Trusts and the majority of primary care practices in the region.
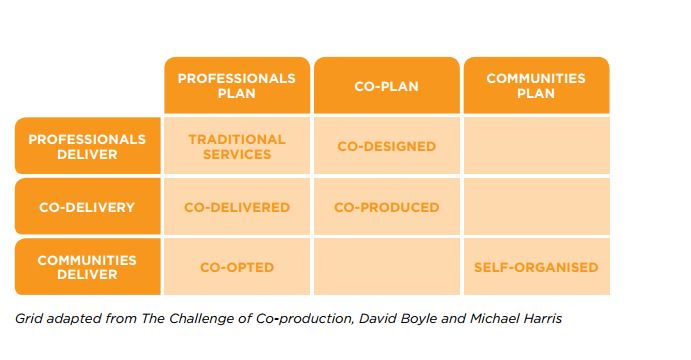
Alongside the creation of 12 Integrated Care Teams, Better Care Together hopes to achieve a transformation in their approach to population health, with primary care and General Practice an important focus, encouraging GPs to host community conversations about wellbeing and how to support it. Community conversations are supported by training on appreciative inquiry and workshops facilitated by the cortia The Art of Hosting which helps to give health and care practitioners and public servants the skills to faciliate better conversations about people's health. These training sessions have involved public sector leaders as diverse as the Chief Constable of Cumbria Police and the Chief Financial Officer of the clinical commissioning group, enabling them to see in practice what Boyle and Harrison (2009) refer to as the 'challenge of co-production'
A better relationship with communities
Local GP Arabella Onslow believe these trainings represent a different skill set to the ones that GPs are equipped with during their training and are usually most comfortable with.
“GPs need to understand that the community looks up to GPs and we have a role whether we like it or not: we need to get better at responding to that”
Arabella believes that one important way to respond to shifting demands is to change perceptions amongst GPs, leading to the recognition that their role gives them significant influence on the health of the whole population which they serve.
Recruiting and retaining highly motivated community-oriented GPs is critical to achieving this. But the shortcomings in the development of the UK’s medical workforce are well known. The General Medical Councils most recent report ‘The State of Medical Education and Practice’ lays out the challenge clearly: ‘We have reached a crucial moment – a crunch point – in the development of the UK’s medical workforce”
Simon Stevens, the Chief Executive of NHS England, responding to this aiming to “pull out all the stops” to increase the number of full time equivalent GPs by 5,000 in the next 5 years, means doubling the recent rate of workforce growth. This is a huge challenge, particularly for places like Morecambe Bay. Indeed across Cumbria in 2016 there were more than 50 vacancies in a consultant workforce of around 200, with critical shortages in acute medicine, paediatrics and other key specialties.
Compounding this is an aging workforce with 20% of GPs aged 55+ and likely to retire over the next 10 years. For the communities around Morecambe Bay, poor accessibility makes recruiting a good stream of locally based GPs more difficult, reinforcing a national imbalance of resources whereby those with most need have the least access to care, which impacts particularly on those in rural areas.
This is a problem that Arabella is acutely aware of, and it also stems from cultural attitudes in the profession:
“People I trained with in London scoffed when I told them I was going to practice in rural Cumbria. I responded by saying: those attitudes are why the inverse care law persists”
Whilst the pressures to the system cannot be ignored, Morecambe Bay is in a good place to scale up innovative approaches with 93% of GP practices within Morecambe Bay recently been rated by the Care Quality Commission (CQC) as “good” or “outstanding”. Indeed, earlier on in the Health as a Social Movement programme we championed a community-led response in Millom which saw groups set up to save local NHS services working with public sector leader to help recruit GPs to their community and in so saved the community hospital that sparked initial protests.
Arabella believes that becoming more focused on population health and better connected to communities might be the key to improving the image of General Practice and inspiring young and socially conscious doctors to enter the profession.
A very General Practice
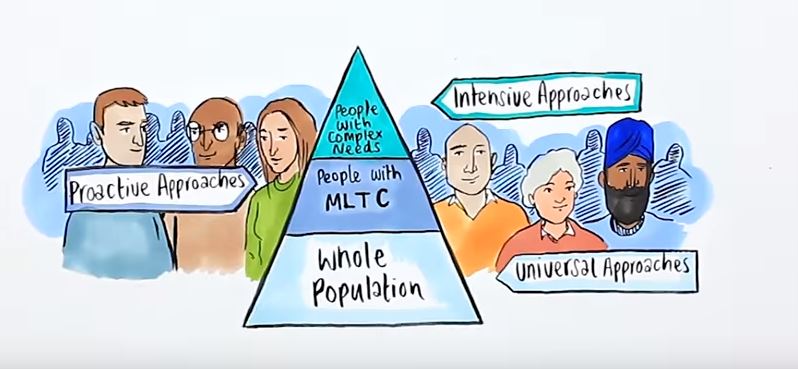
Source: ‘Personalised care for people with long term conditions: A changing GP approach’ NHS England *MLTC refers to Multiple Long-Term Conditions
Across the health and care system there is an acknowledgement that whilst funding remains a critical issue to the recruitment pipeline and addressing retention and overwork, it isn’t the full story. In this op-ed for the British Medical Journal, two medical students call for a shift in the teaching of medicine that combats lifestyle diseases related to diet and nutrition, that some clinicians say is a factor in “up to 80%” of their caseload.
GPs like Arabella are increasingly convinced that the image and practice of these clinicians needs to change. Seeing themselves as community organisers, as well as medical experts, might help GPs reconcile themselves to working with greater complexity without corresponding increase in resource. This would reflect NHS England’s aim to move towards a parity of esteem of "whole population" approches outlined above.
A movement within the medical profession is seeking to match the traditional skills base - devoted to understanding and treating disease - with enhanced skills in developing relationships with patients and the community that focus on wellness. In keeping us healthy long into the future, support for both will be crucial.
Follow @DrBellyButton to find out more about the work continuing in Morecambe Bay and Barrow.
Related articles
-
A social justice cause for the 2020s – reining in health spending
Anthony Painter
Anthony Painter argues that the state expansionists will win over small statists as healthcare expenditure is destined to increase. But their victory may be a Pyrrhic one unless the growth can be limited so better support can also be given to housing, economic security, education and lifelong learning.
-
Did Bevan's bedpan test set the NHS on the wrong track?
Ed Cox
Ed Cox, Director of Public Services and Communities, argues that the NHS needs a more devolved approach in the decade ahead.
-
Self-care doesn't mean less healthcare
Tom Harrison
The need for a healthcare system that prioritises self-care is urgent regardless of austerity.



Be the first to write a comment
Comments
Please login to post a comment or reply
Don't have an account? Click here to register.