The coronavirus pandemic poses unprecedented challenges to science, policy and the interface between the two.
There are growing calls for adaptive leadership in national and global outbreak responses – but what does this look like?
The key is to ensure effective collective decision-making: interpreting harnessing and using the best available emerging evidence, changing trends and shifting scientific understanding, and doing so in ways that help to navigate the considerable uncertainties.
How – and how quickly – policymakers, practitioners and researchers are able to do so in the face of this emerging and complex crisis will make a profound difference to peoples’ lives and livelihoods.
The case for an adaptive response
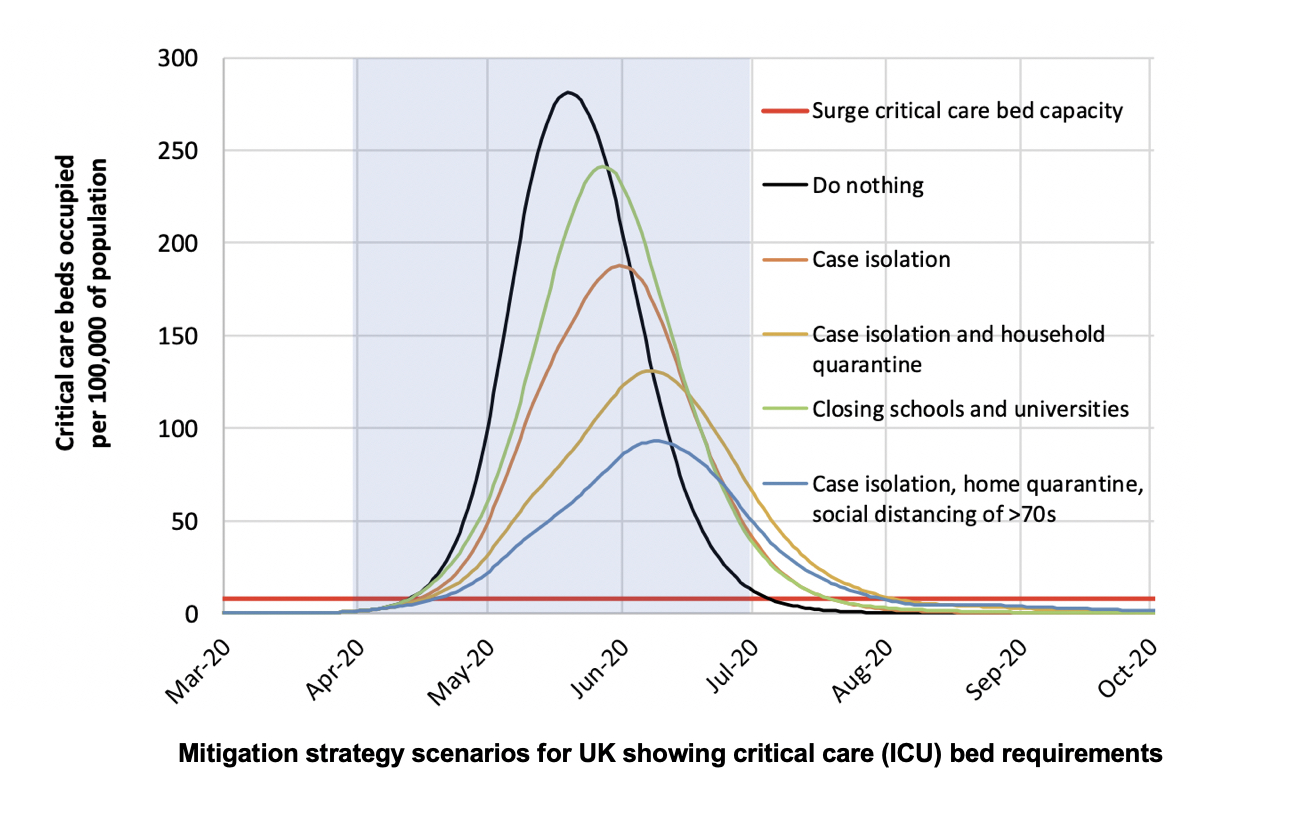
The coronavirus outbreak has already transformed the world in unthinkable ways. It has also shone a light on the power of science to guide decision-making in crises. Detailed epidemiological modelling by Imperial College London helped prompt a shift in the UK, US and other countries from mitigation strategies (allowing a gradual spread of the virus and build-up of the population’s immunity) to suppression – preventing as many people as possible from contracting the disease, and taking steps to delay case number growth for as long as possible; something a number of Asian countries with experience in tackling such pandemics had already adopted. At the heart of the Imperial work is the crucial metric of critical care bed capacity, shown in the chart below.
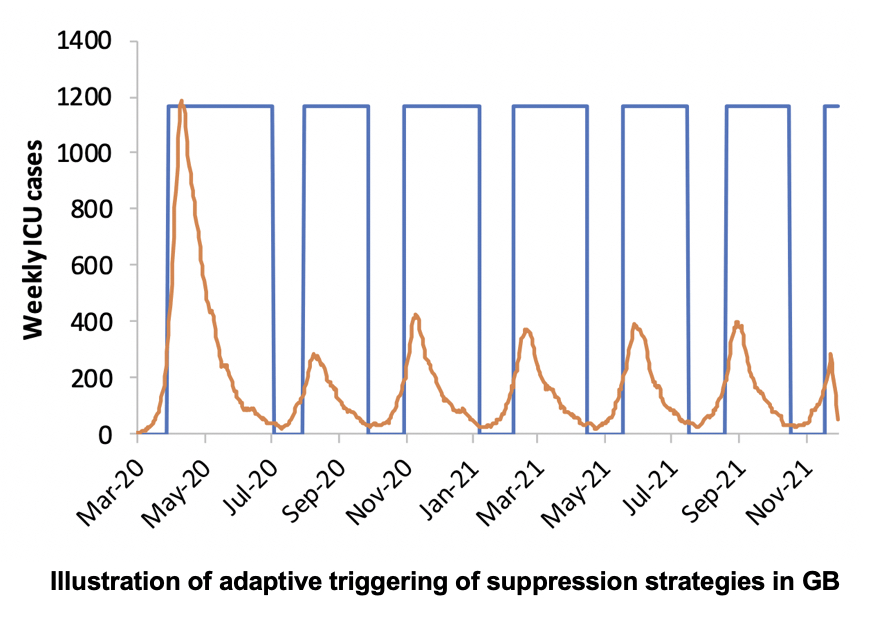
The modelling underlined that the best outcomes would result from a combination of different measures and that very strict initial measures could eventually be relaxed, being reinstated only if incidence increased above a certain threshold (see chart below).
These phases of ‘adaptively triggering’ a set of interventions – switching them on and off, in the popular parlance - could last a significant period. Crucially, this would help buy time to learn more about how best to treat, respond to and hopefully vaccinate against COVID-19. Scope to trigger and relax different sets of interventions could arguably be even more important in low income countries, because of the risks of already weak health systems becoming rapidly overwhelmed and some of the challenges of enacting some measures (for example, social distancing is much harder in areas which are densely populated and which lack infrastructure to ensure people can access what they need from home).
Applying adaptive management in practice
While the arguments for such an adaptive approach are clear, the concept of adaptation set out in the Imperial work reflects a theoretical approach, akin to the outbreak response effort being a giant thermostat controlling the behaviour of entire nations, with different interventions switched on and off as needed, much as one might turn the heating on and off.
What we see as ‘adaptive management’ is grounded in evidence and learning from many different efforts, including natural resource management, military planning, international development and humanitarian responses.
It means the collective ability to learn about the delivery of interventions, to identify which different interventions - or combinations of them - might work best, and why, as well as understanding the impacts of these interventions.
This style of adaptive management has recently gained traction in disease outbreak management, most notably in response to Ebola in West Africa. Numerous analyses of the successful eradication of small pox also show that the success was attributable, more than any other single factor, to processes of strategic adaptation and learning.
Adaptive management of this kind can address an important criticism of model-based learning, which might focus only on epidemiological factors (transmission rates, etc), and assume operational responses have complete control – for example, that the public follows the proscribed rules, that drugs are delivered on time, that beds become available when needed, and so on.
Experience has taught us the hard way that such assumptions often do not match up to reality, and the resulting interventions seldom proceed as planned. Instead, we need to think about our strategies as ‘designed and intended to adapt to change’.
Our work suggests policymakers, researchers and practitioners working on the ongoing response should consider the following questions to establish ‘adaptation by design’ in responding to the current crisis:
- Why we need to adapt? Frame the case for adaptive changes with a clearly communicated objective e.g. to minimise total deaths, address risk of exceeding health-care capacity or alleviate indirect economic hardship.
- What we need to adapt? – Make clear from the outset the specific elements of the response that may be changed, for instance reducing some interventions while keeping others or changing how a particular intervention is delivered.
- How we should adapt? – Advocate for an objective and transparent system of governance that reviews evidence and communicates the argument for changes to interventions. This needs to be based on ‘candid, trustful relationship[s] which facilitates the acceptance of the new’ between policymakers and a range of different kinds of experts.
- The evidence base needed? Identify key information and data that can be used to inform decision-makers and other stakeholders on all of the above (e.g. numbers of cases, feedback from frontline staff and local authorities, evidence from other countries, etc.).
Towards adaptation by design
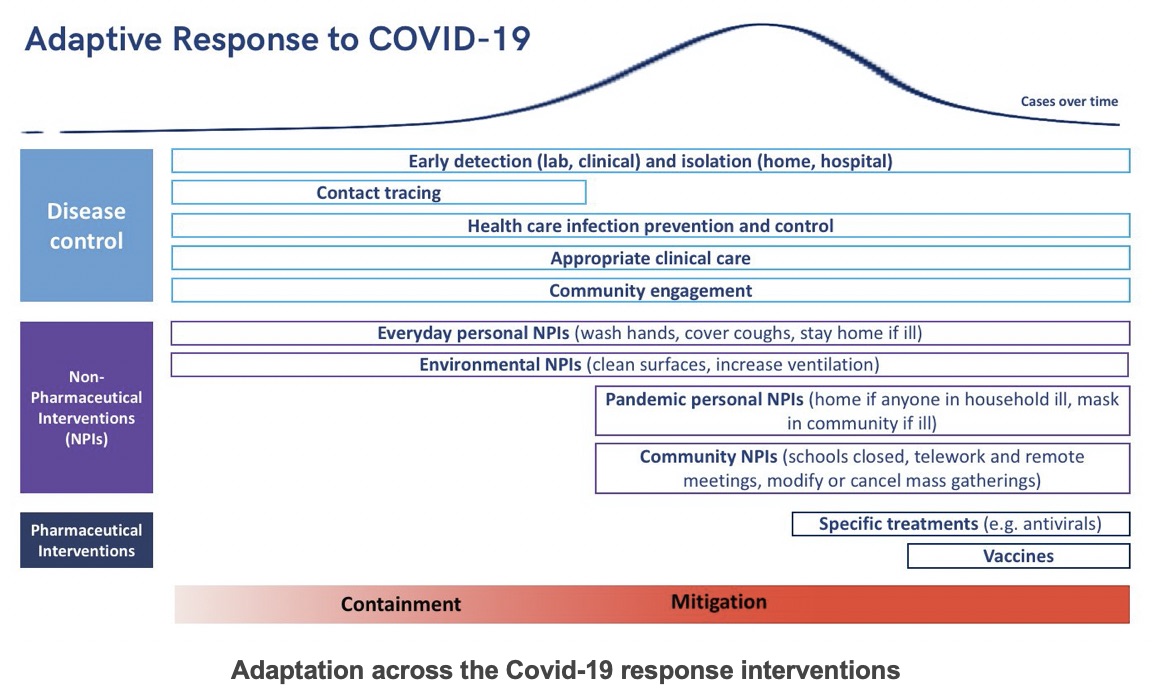
‘Adaptation by design’ means developing and communicating a process that recognises interventions need to change and adapt as we learn more, and establishing clear processes for collecting, interpreting and acting on evidence. A former Director of the US Centre for Disease Control has usefully set out the range of different interventions that need to be considered in an adaptive response (see chart below) and has argued for the response to ‘learn intensively [using] real-time data’.
Based on our work, this means identifying the information of most value to decision makers and using this to set out an agreed approach to how learning will inform different kinds of decision making.
Quantitative and qualitative scientific analysis such as mathematical modelling, ethnography, behavioural science and more can all help to evaluate different sources of uncertainty across these interventions. They can be used to underpin evidence-based ‘triggering’ of intervention changes as evidence is gathered and gaps in understanding are filled.
This helps to address a key challenge faced in epidemic management, namely accepting, and formally accounting for, the evidence base’s limitations.
While many governments are rightly stating their commitment to ‘follow the science’, there is not (yet) any definitive evidence or agreed scientific base to guide current decision making; hence, the differing policy responses in different countries, reflecting their own interpretation of this evidence, and of their capacities, sociological features and more.
Rather than imagining there is a perfect solution, policymakers will need to continue to rapidly interpret different forms of evidence and data and make ongoing judgement calls based on their best interpretation.
At the same time, policymakers in each country need to determine exactly what they are trying to achieve - ‘minimising the impact of the outbreak’ is easy to say, but means very different things to different people (e.g. what emphasis is placed on reducing overall number of cases, economic impacts, social impacts and so on).
The variation in national response strategies presents an opportunity to learn from each other and rapidly adopt/emulate/remove policies that have been successful or sub-optimal elsewhere. Such an approach makes a strong case for the role of international communication and transparency among national actors too.
A roadmap for adaptive management of coronavirus responses
An adaptive management approach will require a number of key steps. Based on evidence-informed adaptive management in development and humanitarian contexts, we set out the following steps for the COVID‑19 response:
- Defining a set of key measures/metrics that could be used to identify triggers of changes to interventions. These could reflect evidence of further spikes in cases, increasing mortality rates, overstretched health care capacity, as well as measures of ‘community resilience’, strength of local support networks, evidence of social or psychological impacts and so on.
- Collect a range of operationally relevant data and evidence, while being realistic about the need for ‘quick enough’ and ‘good enough’ measures, given quickly changing trends. Alongside vital clinical data, tapping into networks that can quickly gather and share feedback at different levels and scales of the response -from health professionals, public officials, police officers, community organisers and so on - could be key in providing a ‘temperature test’ for key pressure points.
- Ensuring that evidence is robustly assessed. Interpreting evidence from a range of different perspectives - medical, social, behavioural - will be essential for ensuring all aspects of the response are properly considered, and ultimately a set of judgements have to made based on the best evidence available, collectively, with inputs from a range of perspectives.
- Finally, this process of interpreting evidence and agreeing to a set of triggered actions should all be well documented, and made as transparent and inclusive as possible. Given the inevitable variation in interventions, implementation and outcomes across communities, transparent processes of interpretation and learning will help to minimise decision-making biases and help to minimize anxiety and facilitate engagement of the diversity of affected communities and groups (including different age groups, ethnicities, regions and more).
Building adaptive leadership capacities
This cannot just be seen as a technical endeavour. As noted by David Nabarro, the Special Envoy to the World Health Organization Director-General on COVID-19, adaptation to coronavirus is a leadership imperative, especially at the scale that the pandemic response demands. We identify a number of key capacities for enabling such adaptive leadership, which align closely with the RSA’s core change model to ‘think like a system and act like an entrepreneur’. These are as follows:
1. Build leadership vision and a supportive management culture across the different teams and units coordinating the response
Decisions on when and how to trigger a change in response cannot be made by a small number of people behind closed doors. This is not the usual mode of operating for many governments, and means being transparent about what is being learnt and when shifts in action and interventions will be needed to ensure their effective delivery.
2. Think beyond specific interventions towards the whole system
A whole-of-system perspective is needed to understand how best to calibrate interventions. This means ongoing assessment of how interventions are working, making changes to their delivery where gaps are identified, as well as continual review of wider system effects (such as how can communities be supported to become more resilient, especially when faced with knock-on impacts such as breakdown of other key services ordisruption to supermarket suppliers).
3. Encourage and join-up locally led innovation and problem solving.
Many countries have already seen a proliferation of community-led support initiatives, organised at the very local level. These are likely to be key to catalysing changes in behaviour that will need to be maintained longer term, including ensuring that physical distancing does not mean social isolation. These are by their nature hard to predict and plan for - but their emergence will need to be anticipated and incorporated into dynamic learning processes. Strong facilitative leadership to encourage transparency about these efforts, to embrace learning from both successful and failed efforts, is critical to maximising societal benefit.
4. Envision the future
The coronavirus pandemic has shown all too clearly how interconnected and interdependent we are. What we do in this crisis response will have repercussions – direct and indirect - for years and decades to come. This too will demand systemic and adaptive leadership, to help us think beyond the shadow of the pandemic to the kind of world we want to forge together.
Ben Ramalingam is a senior research associate and Leni Wild is a senior researcher with the Overseas Development Institute in London, UK.
Matthew Ferrari is a professor at the Center for Infectious Disease Dynamics, The Pennsylvania State University, Pennsylvania, USA.
Comments gratefully received from Matthew Taylor, Emma Proud, Alex Roberts and John Atkinson.
A longer version of this piece is available on the Overseas Development Institute website.
Related articles
-
Covid-19: A ‘year of stabilisation’ to build bridges to the future
Matthew Taylor Anthony Painter
3 principles and 10 ideas for transition.
-
How to create real, lasting change after Covid-19
Ian Burbidge
We must look for the potential of change in the crisis response. The post-crisis task is to find ways to amplify and embed the most promising changes and innovations.
-
The path from crisis
Matthew Taylor
The Covid-19 pandemic is generating momentum for change in many parts of society. But perhaps the biggest shift of all would be an appetite for new leadership.




Join the discussion
Comments
Please login to post a comment or reply
Don't have an account? Click here to register.
Really strongly agree with this systems approach and the need for responses that are agile and adaptive .
We need to encourage and enable agile speedboats rather than top down steam ships . Check out an article I posted on this subject in vulnerability 360 website
I received good advice on Complex Adaptive Leadership from Nick Obolensky - highly recommend getting in touch with him via LinkedIn.